I offer my patients safe, effective, and predictable shoulder replacement surgery.
The prosthesis I use for shoulder replacements is either the Lima SMR, or Equinoxe from Exactech. In the past I have used the Zimmer prosthesis as well.
What is shoulder replacement?
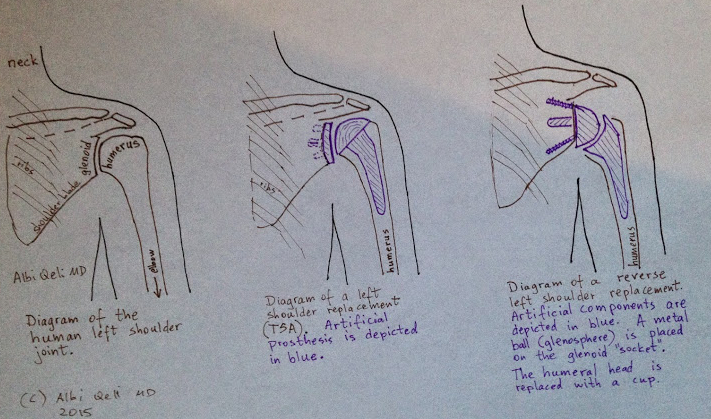
Several different operations are labelled "shoulder replacement," so it is important to know the difference.
- Total shoulder arthroplasty (TSA) implies replacement of both sides of the shoulder joint, the humeral head, and the glenoid socket.
- In reverse replacement (RSA) the ball and socket switch places. A metal ball is placed on the glenoid, and a socket replaces the ball of the humerus. It is a better type of shoulder replacement when the rotator cuff is dysfunctional, or is expected to be dysfunctional.
- Hemiarthroplasty is a partial replacement. Only the ball (of the ball-and-socket) is replaced. The glenoid (the socket) is left alone. This operation provides less reliable pain relief, but it avoids dealing with what is an unsolved problem in shoulder replacement surgery: poor glenoid bone stock.
- Surface replacement is a type of hemiarthroplasty (see #2 below). The difference with traditional arthroplasty is that the humeral component does not have a stem that goes down the humerus.
How is the surgery done?
As a patient, you need to know that shoulder replacement requires the use of power tools and hammers, and therefore there is some inherent risk.
I approach the shoulder joint from the deltopectoral interval, which is a proven, safe, work-horse approach to the shoulder. I then use a chisel to perform a lesser tubercle osteotomy in cases of primary shoulder replacement. I use a power saw to remove the humeral head. I use power reamers to prepare the glenoid (socket). Hammers are used to insert the artificial components. Typically I do not use cement, as the Lima SMR shoulder prosthesis works well without cement.
What are the risks of shoulder replacement?
- Death. Even before surgery, the anxiety surrounding the operation may precipitate a heart attack and death. During surgery, general anesthesia may precipitate a heart attack, stroke, etc. After surgery, pain, pulmonary embolism, infections, etc., may precipitate heart attacks and death.
- Postoperative infection. A deep prosthetic joint infection requires additional surgery. Deep prosthetic joint infection is usually treated with removal of the artificial prosthesis and prolonged injection of antibiotics. Reinsertion of a prosthesis may be done after the infection is cleared. The risk of a periprosthetic infection is approximately 1%. Periprosthetic infection may result in a permanently removed prosthesis, known as resection arthroplasty.
- In the immediate postoperative period after TSA, one must allow enough time for the subscapularis tendon to heal. In order to reach the shoulder joint during surgery, the subscapularis tendon must be detached from the humerus, and this must be then reattached at the end of the operation. It takes approximately 6 weeks for this to heal.
- Glenoid loosening remains a weak point in shoulder replacement surgery.
- Rotator cuff disease can coexist with glenohumeral arthritis, and progression of rotator cuff disease may cause development of pain, even after a shoulder replacement. Progression of rotator cuff disease may need to be treated with conversion to a reverse shoulder replacement prosthesis.
- Nerve damage is possible due to the proximity of the shoulder to the brachial plexus and in particular the proximity to the axillary nerve.
What is the typical recovery after this surgery?
- Patients typically spend one night in the hospital after surgery
- Initial rehabilitation for 6 weeks without active subscapularis firing
- Full rehabilitation and strengthening between weeks 6 to 12 after surgery
- Activities such as contact sports are not allowed after shoulder replacement.
Case study: regular shoulder replacement (TSA)
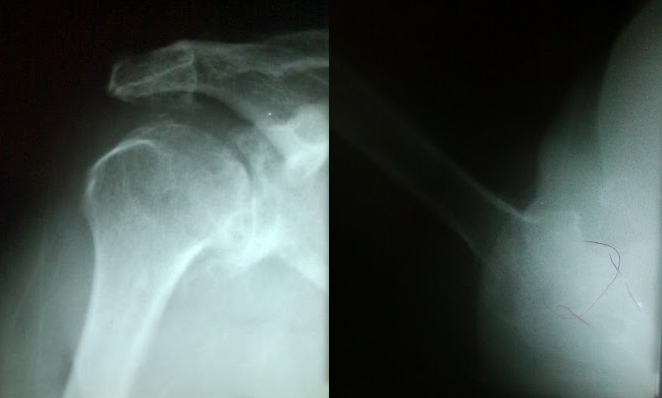
60-year old female with severe right shoulder arthritis, severe pain, stiffness, and grinding. On presentation, she was able to forward flex her shoulder only about 45 degrees, and with severe pain.
In the xrays below, note the irregular appearance of both the glenoid and humerus, the inferior ostephyte, and the degenerative cysts.
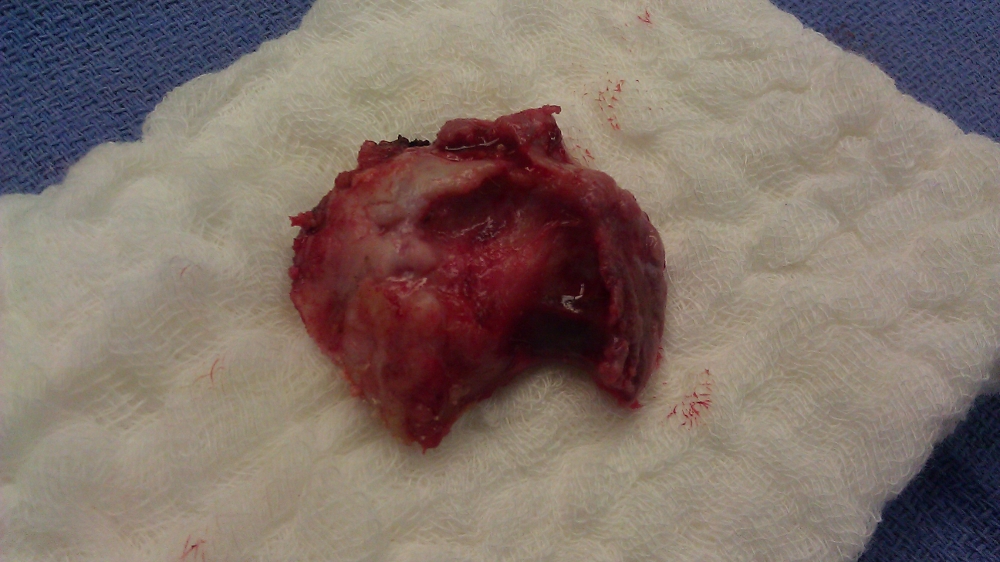
Below is a picture of the deformed head of the humerus that was removed during surgery. This was accomplished with a motorized power saw.
Below are xrays after surgery. This is a typical appearance of a shoulder replacement on xray. This is the same patient picture above, 3 years after her right shoulder replacement.
This prosthesis is the Exactech with a 38mm head.
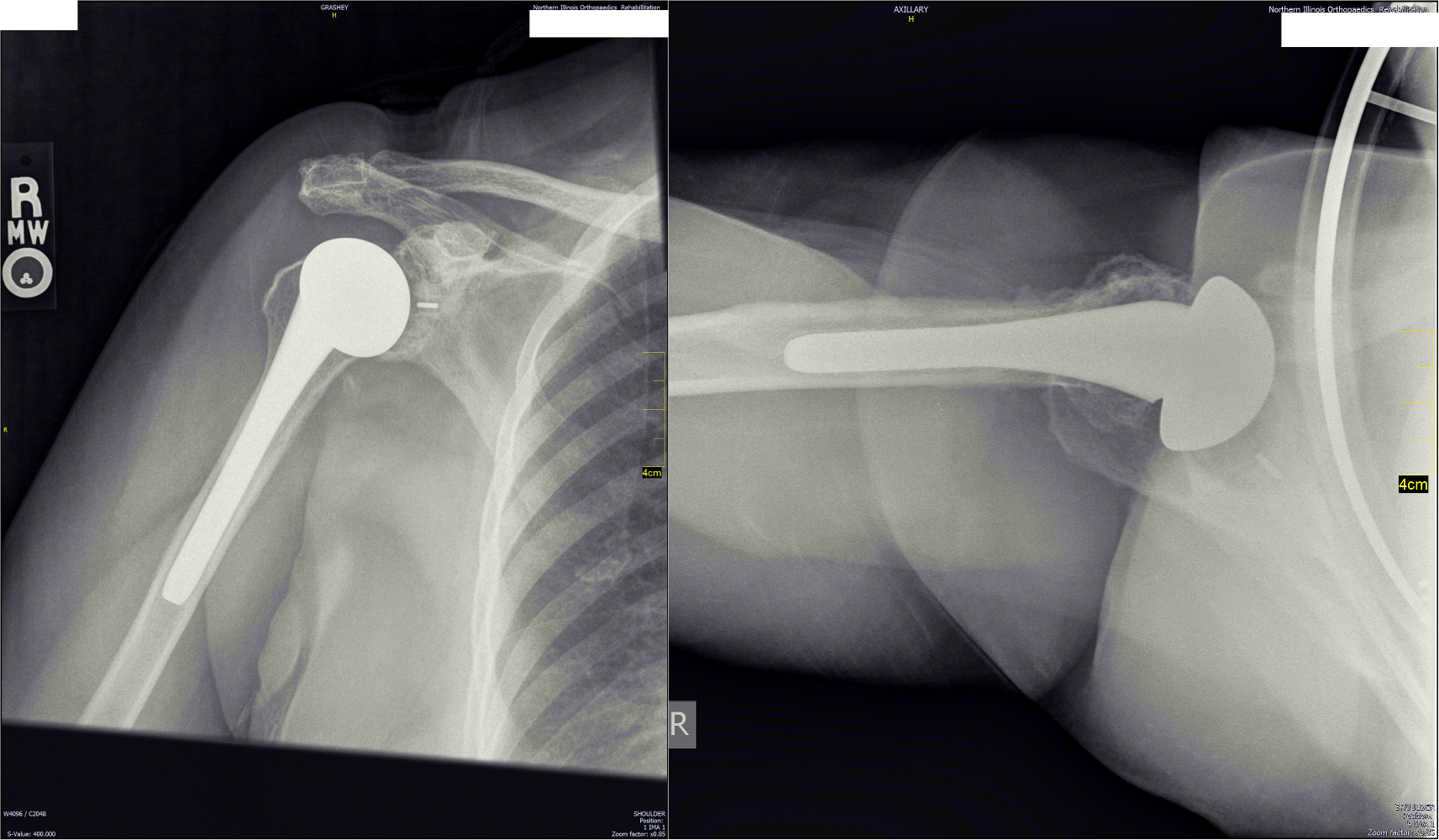
With a good repair of the subscapularis, it is possible to get full motion of the shoulder after the surgery.
