Hip replacement is an operation during which a dysfunctional hip joint is replaced with an artificial implant.
Who should get a hip replacement?
A hip replacement is the correct operation when the hip joint is worn AND the pain from the "bad" hip joint is severe.
It is possible to have an arthritic hip that does not hurt a lot. It is also possible to have a very painful hip where the cause of the pain is soft tissue injury, a bad back, and so on. In the latter circumstances, the hip replacement operation is probably not the correct medical intervention.
How is the hip replacement operation done?
The hip replacement operation is performed using power tools, chisels, and hammers. The operation looks very violent to the untrained eye.
These are the surgical steps for a hip replacement operation.
- Spinal anesthesia is the way to go. If effective spinal anesthesia cannot be achieved for whatever reason, then general anesthesia is an option.
- Approach: there are several different ways to surgically approach the hip joint. Each method has advantages and disadvantages.
- After the hip bones are exposed, a power saw is used to cut and remove the femoral head.
- The acetabulum socket is then reamed with a power reamer.
- A shell is then impacted in the prepared acetabulum.
- A liner (also known as a bearing) is impacted inside the shell.
- The femur is then milled to accept the prosthetic stem.
- The prosthetic stem is then impacted, and the head is installed on top of the stem.
- The wound is then closed.
Which is the best hip replacement prosthesis?
In the US market there are multiple successful hip replacement prostheses. I use the Corail/Pinnacle prosthesis, usually with a ceramic head on highly cross linked UHMW polyethylene bearing. This is a device with an excellent track record.
Here's a picture: on the left are the separate components, which are assembled on the right.

The big 3 hip prosthesis makers in the US are Zimmer, Depuy, and Stryker. Each manufacturer offers different prosthetic options. Even within a single prosthetic line, each manufacturer offers different bearing types, from polyethylene, to metal, and ceramic.
The manufacturer of the hip prosthesis that I use is DePuy, a J&J company. Like the other orthopedic manufacturers, DePuy markets several different lines of prostheses, some of which have had problems. As I explained above, the Corail hip system remains an excellent choice, and has had an excellent track record for close to 30 years. I've personally being implanting it in my patients since 2009.
What is the typical course after hip replacement?
- Usually discharge home on day 1 after surgery.
- Initial healing lasts 6 weeks, full healing takes approximately 6 months
- No driving for the 1st 6 weeks after surgery
- Discontinue walker and crutches by 2 weeks, may use a cane if necessary
- Discontinue cane by 4-6 weeks.
- Discontinue all pain medications by the end of the month.
- It is prudent to follow dislocation precautions for the first 6 weeks after surgery.
- Follow up routine for my patients
- 2 weeks for staple removal
- 6 weeks, with X-rays
- 3 months, 6 months, 12 months, with days
- Yearly thereafter, to check for mechanical wear.
- Lifelong use of prophylactic antibiotics before dental procedures (there is controversy regarding this recommendation).
What are the risks of hip replacement surgery?
Hip replacement is routine operation, but it is not risk free. As a patient you must understand these risks. If these risks are not acceptable to you, you should not have this operation.
Death
The risk of death from a heart attack increases with age. Therefore, patients who seek joint replacements have an inherently increased risk of heart attacks.
- Even before the hip replacement, the anxiety surrounding the operation may precipitate a heart attack and death.
- During surgery, general anesthesia may precipitate a heart attack, stroke, etc.
- After surgery, pain, pulmonary embolism, infections, etc., may precipitate heart attacks and death.
Leg length difference
For conventional hip replacement surgery, with the patient positioned on the side, up to a half inch leg length difference can be expected. Usually it's much less and not noticable.
Fractures
Please keep in mind that power tools and hammers are used routinely during the operation. Fractures do happen occasionally, most are not mechanically significant and weight bearing without restriction is often allowed.
DVT and PE
Deep vein thrombosis is a well known complication and a leading cause of death after major surgery in the US. DVT may lead to PE, and a big enough PE may cause sudden death. However, most patients who suffer from thromboembolic disease do not die from it.
Unfortunately, the medical profession does not have a full understanding of this important issue. There is an important element of "bad luck." Do inform me and other health care professionals involved of any history of embolism that you may have.
The current state of affairs is such that most physicians recommend using anticoagulant medications ("blood thinners") after the operation, in order to decrease the chance of getting DVT or PE. It could be aspirin (the mildest,) Coumadin (a very fussy medicine,) or Lovenox (which requires daily injections). By their very nature these medicines can cause additional bleeding. Duration of such preventive treatment is controversial.
Infection
Infection affects approximately one in 100 patients with a hip replacement. Cure usually requires removal of prosthesis (a second surgery), IV antibiotics for 6 weeks, and delayed reimplantation of the hip prosthesis (a third surgery). In other words, an infection makes for a very unpleasant half year or so. During that time it may be difficult to get around without a wheelchair.
Dislocation
Dislocation occurs when the artificial ball of the prosthesis disengages from the artificial cup.
Together with infection, dislocation is one of the two main orthopedic complications after a hip replacement operation. In other words, when a hip replacement operation has to be redone, it is usually either due to an infection or due to dislocation.
Statistically, the posterior approach surgery has a higher risk of dislocation. In addition, certain diseases, such as Parkinson's, are associated with a much higher risk of dislocation after a hip replacement.
The direct anterior approach diminishes the risk of dislocation. The anterior approach is described in a separate file, but the main point is this: it decreases the risk of dislocation associated with the posterior approach, it avoids the limping of the anterolateral approach, at the cost of being a bit more demanding for the surgeon.
Nerve damage (foot drop)
The risk of having a foot drop after hip replacement is approximately 0.5%, that is to say, out of 1000 patients with hip replacements, 5 have some degree of visible foot drop. The reason for developing foot drop is unclear most times. Most patients with foot drop after hip replacement have preexisting spinal stenosis and a certain predisposition for developing this problem.
Foot drop complicates rehabilitation after hip replacement, but prompt fitting with an AFO can mitigate the problem. Roughly half of patients improve and become able to dorsiflex the ankle, but it can take a year or more.
Are there alternatives to hip replacement?
Nonsurgical alternatives to hip replacement
- Weight loss.
- Avoidance of painful moves, activities.
- Pills, typically antiinflammatory medications. This group of medications includes tylenol, ibuprofen, naproxen, mobic, indomethacin, etc.
- Physical therapy.
- Cortisone injections of the hip.
- Using a cane or walker.
Surgeries other than hip replacement
- Removal of osteophytes arthroscopically: may provide some relief in early stages of arthritis, but efficacy remains unproven. You may wish to try this operation anyhow, if you do not feel ready to have a hip replacement.
- Osteotomy: a major operation, yet results are not reliable. In addition, an osteotomy operation may make a subsequent hip replacement more difficult. There is a role for acetabular osteotomy in patients with dysplasia, however.
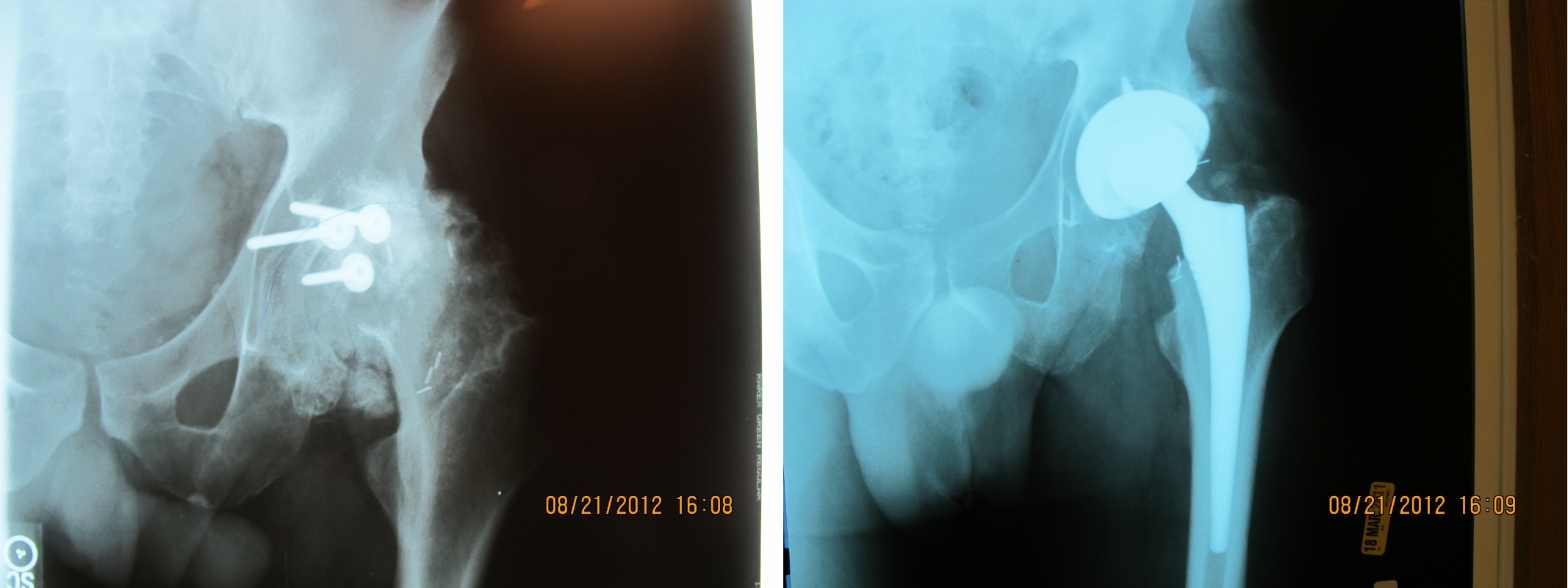
Case study: a 40 year old with posttraumatic arthritis
The xrays are from a 40 year old patient who had sustained a posterior acetabular wall fracture. His initial injury had been treated surgically at a major university. Unfortunately, the nature of such injuries is such that most of them develop arthritis despite prompt appropriate care. Two years after his acetabular fracture surgery, his left hip joint is as arthritic as can be. The xray to the right shows the implanted DePuy Corail/Sector hip prosthesis. This solved his pain problem and restored normal gait.