A hip replacement prosthesis can fail for various reasons. A redo operation is known as revision hip replacement.
Statistically speaking, today (2016) the 3 most common reasons for failure of a hip replacement prosthesis are
- Infection
- Dislocation
- Adverse reaction to a metal-on-metal prosthesis: pseudotumors, local tissue damage, cobalt poisoning, etc.
In my own practice, in the first 7 years I had performed more than 300 hip replacements, and I have had to revise just one back in 2010, for infection two of them, one for infection in 2010, and one for dislocation in 2015.
What are the risks of revision hip replacement surgery?
Revision of a hip prosthesis is not a trivial operation. All the risks of regular hip replacement surgery apply: a patient undergoing revision surgery is presumably aware of such risks. However, both the rate of complications, and the severity, are increased compared to a regular hip replacment.
Depending on the situation, the entire prosthesis may have to be removed. Certain prostheses are notoriously difficult to remove: the femur typically has to be osteotomized to allow removal of the stem. Recovery, as a consequence is slower as well.
The following cases illustrate some of the points above.
Case study: infected hip prosthesis
This patient had had a hip replacement operation in order to treat a hip fracture in Guadalajara, Mexico. He was living with his daughter in the US, still unable to walk, more than a year after his fracture.
Xray appearance and blood tests indicated a low grade infection of the left hip prosthesis. A needle aspiration of the hip joint showed that he was infected with Streptococcus spp bacteria.
Faced with a deep infection of a prosthetic joint, standard treatment in the US consists of two stage revision. Here's what this means:
- A first surgery to remove the infected prosthesis and to mechanically remove as much of the infected tissues as possible. An antibiotic spacer, which may or may not allow the patient to bear some weight on the hip, is usually inserted.
- Antibiotics by IV for at least 6 weeks.
- After the infection is cured, a second surgery to insert a new hip prosthesis.
This treatment plan has an approximately 80% long-term success rate.
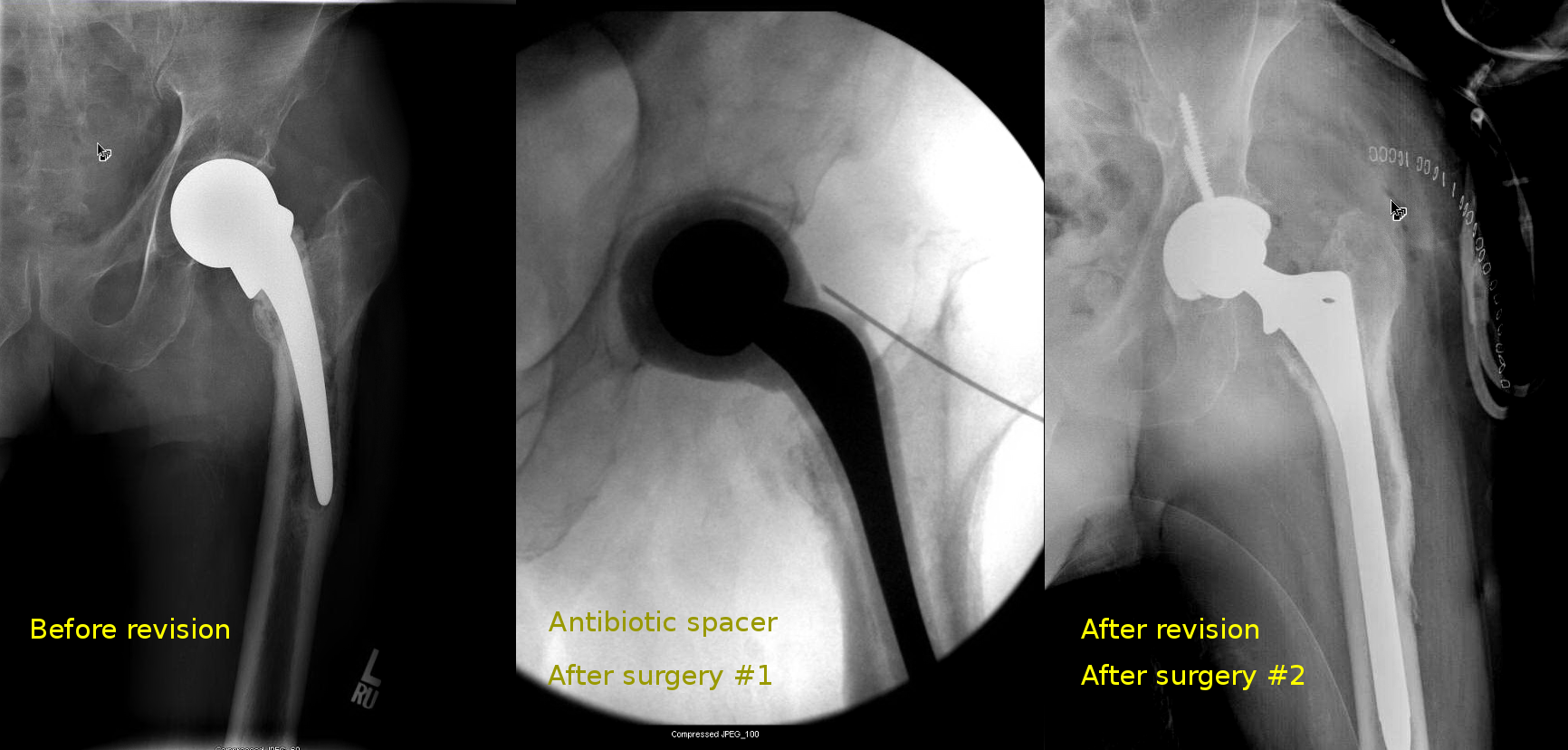
In this particular case, it was fortunate that the entire implant came out easily together with the cement mantle. In many cases it is necessary to perform an extended trochanteric osteotomy to remove the implant (see another case description below).
Patient became able to walk and stayed clear of infection when I last saw him, more than 3 years after surgery.

Case study: revision of a metal-on-metal prosthesis
As of 2016, I have revised a handful of metal-on-metal hip replacements, with good success. This case is interesting because it is a case of hip resurfacing, the so-called Birmingham hip replacement, which developed a pseudotumor and pubic rami fracture. The pseudotumor can be clearly seen in the xrays, and the blood metal ion levels were very high.
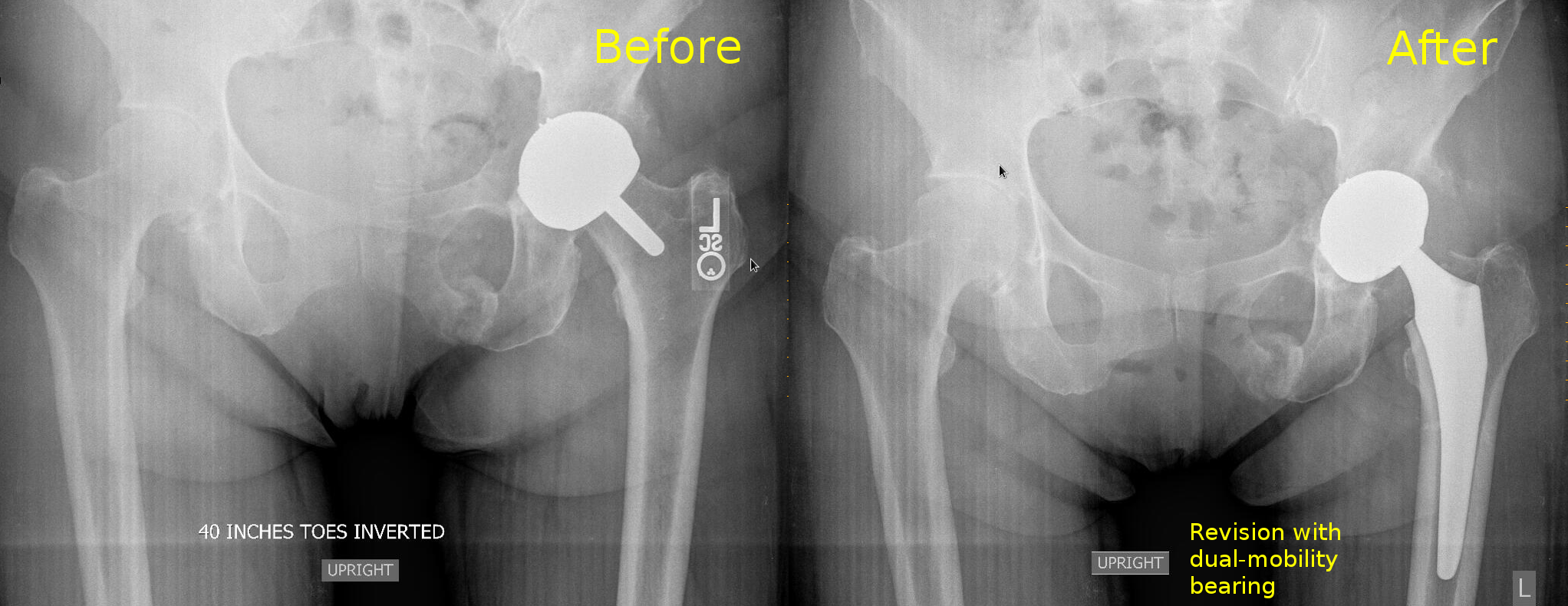
I typically revise the metal-on-metal prosthesis, if possible, by changing the big metal head into a dual mobility bearing. This avoids a femoral osteotomy, and resolves the issue of the metal-on-metal bearing.
For this patient, after revision as above, the metal ion levels came down and the pubic rami fractures healed.
Case study: revision of old cemented prosthesis
Prior to the advent of highly cross-linked polyethylene, the plastic bearings were prone to formation of microparticles that resulted in bone loss around the prosthesis (known as osteolysis). If you are a patient with an old hip replacement, you ought to have it checked every few years just for that reason.
This particular hip prosthesis had functioned well for more than 20 years before it started failing. The patient started feeling severe pains, more intense and more frequent with time.
Xrays show an old style cement job, a failing prosthesis, with osteolysis, debonding.

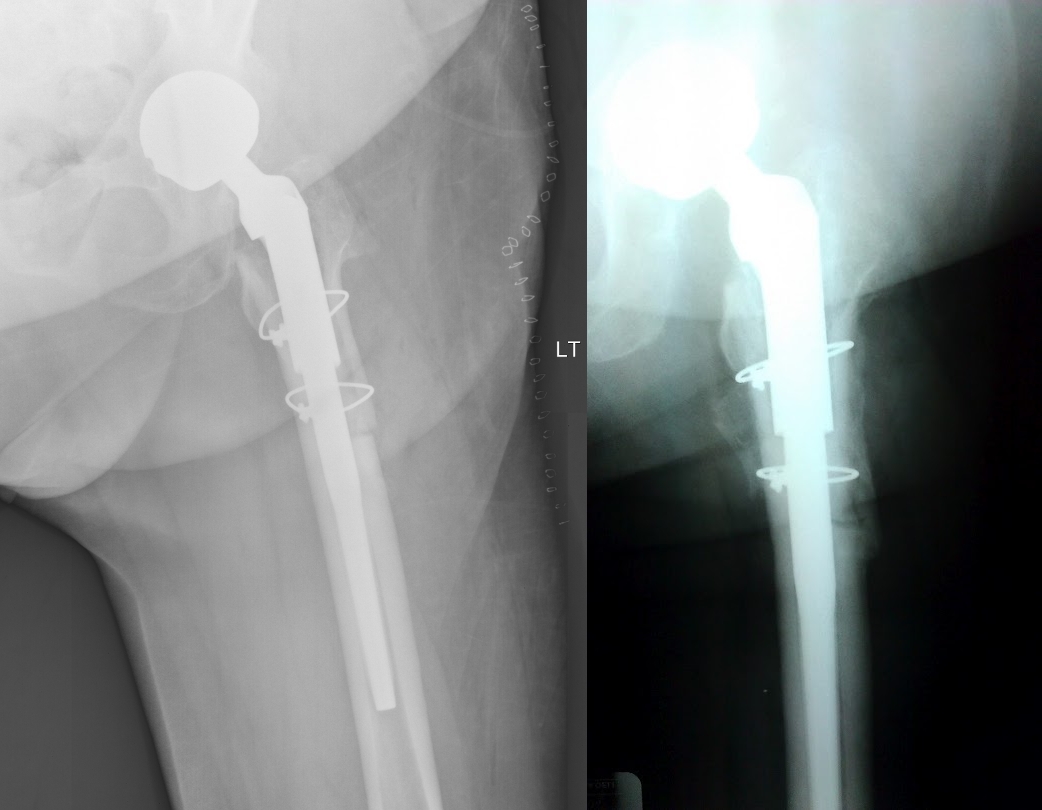
Revision of this type of prosthesis requires removal of the old hardware, including removal of the old cement from inside the femur. In order to do this, an extended trochanteric osteotomy is necessary. This is a procedure whereby the femur bone is cut with a saw lengthwise, and then the canal is opened and scraped. The bone is afterwards repaired with circular wires.
A new prosthesis is then inserted.
This type of operation is very painful, and inherently risky.
Following this operation, the femur bone has to be allowed to heal in order to fully support the new prosthesis. Therefore, weight bearing is initially limited.
This is what the revised prosthesis looks like:
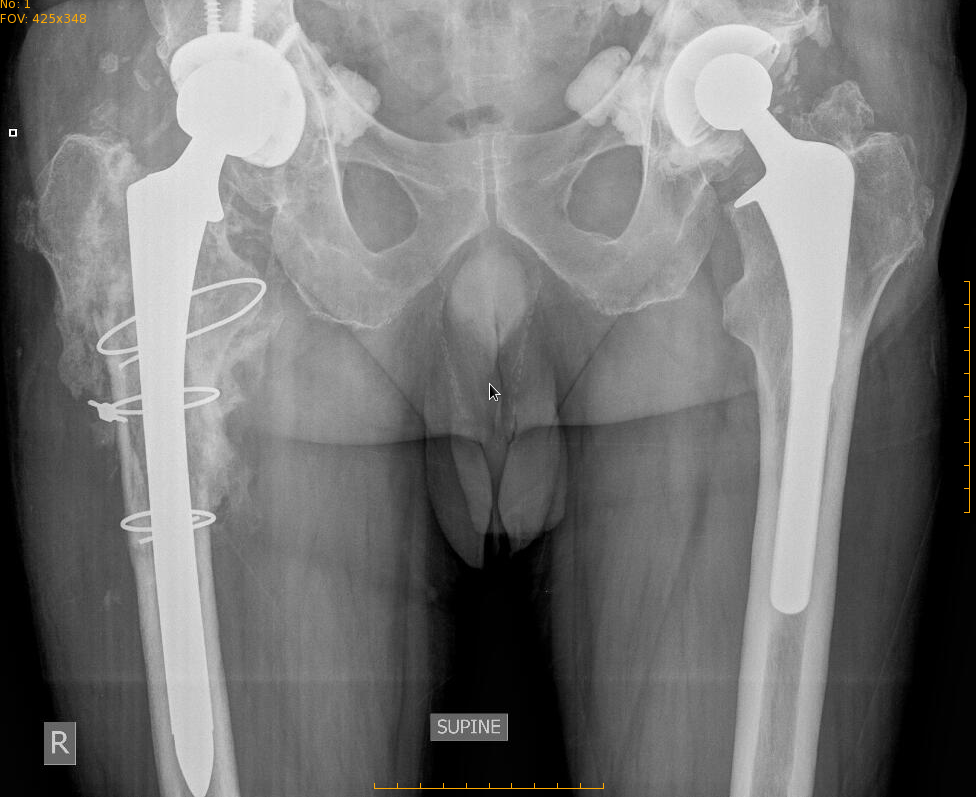
This patient healed in due course and became able to walk without pain.
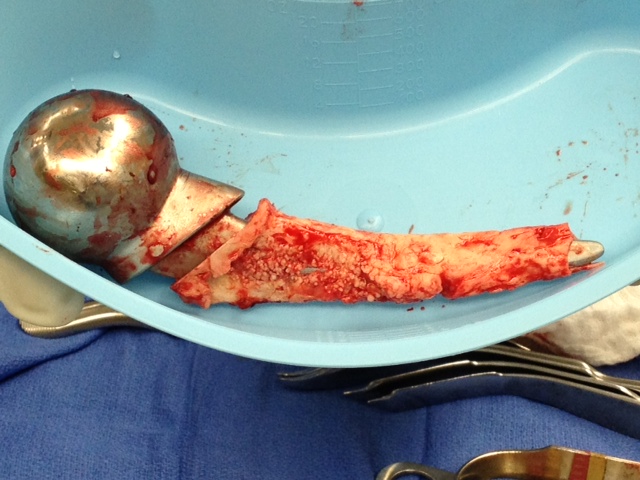
Case study: mechanical failure of the prosthesis
This is the case of a patient who had had a hip replacement elsewhere, with a "new" prosthetic model. This particular prosthesis featured a large metal-on-metal articulation, as well as a modular neck-stem junction.
Patient was satisfied with her surgery until one day she was walking on it, and it suddenly "snapped."
The modular neck of the prosthesis had failed, was broken in two pieces. Just like that.
This is what it looked like after removal from the patient.

Removal required an extended trochanteric osteotomy. In other words, using a saw, a bur, and chisels, the femur was fileted open and the metal prosthesis was hammered out.
Xray above shows the new prosthesis immediately after surgery, and 3 months later.
This patient went on to heal the osteotomy and did well. She became able to walk without a limp, pain free.
Cases like these serve as acute reminders that one must very carefully consider the use of "the latest and the greatest" implants and one must respect the old prostheses with established records. (Or in the words of one of my orthopedic colleagues "Avoid the new implants like the plague.")