Performing the hip replacement operation from the anterior approach has a few advantages.
- It allows the surgeon to do X-rays during surgery. This helps make sure the components are well positioned and leg length is accurately restored.
- Allows surgeon to preserve posterior capsule and muscle, decreasing risk of dislocation.
- Allows surgeon to preserve hip abductors. Dysfunction of the abductor would cause prolonged, if painless, limping.
What are the other approaches to the hip?
In order to perform a hip replacement, the hip joint can be approached in several different ways:
- Transtrochanteric approach
- Posterior approach: also known as transgluteal approach, as well as posterolateral approach.
- The anterolateral approach: also known as the lateral approach, or sometimes as the Hardinge approach.
- The direct anterior approach, known also as the Smith-Petersen, or Hueter approach.
A little bit of history
Hip replacement operations have been done successfully since the 1960's. Dr John Charnley, in England, was the first to routinely perform successful hip replacements. His basic idea remains valid to this day: a metallic ball that articulates with a polyethylene socket.
His approach to the hip was transtrochanteric. He performed an osteotomy of the greater trochanter of the femur in order to get into the hip joint. After the surgery, the osteotomized trochanter had to heal.
Glossary
Osteotomy = Cutting of bone. This is done with saws, chisels, and other such tools. Trochanter = rough prominence of bone in the femur that serves as attachment for the hip abductor muscles.
Current artificial hip joints are similar to those first implanted by Dr Charnley in that they are made of a metal ball and a polyethylene socket. However, the method of insertion is rarely the same. Although a trochanteric osteotomy is sometimes needed for a revision surgery, an uncomplicated hip replacement is nowadays almost never done via an osteotomy. Instead the surgeons go either in front or behind the trochanter of the femur. The two common current approaches therefore are the anterolateral or Hardinge approach, and the posterior approach.
What is the problem with the posterior and with the anterolateral approaches?
The posterior approach is a very good approach, in that it preserves the hip abductors and does not cause as much limping as the anterolateral approach. The posterior approach is very popular among US surgeons. I personally am very familiar with it, and in fact it is my approach of choice for doing a quick hemiarthroplasty in elderly femoral neck fractures. The problem with the posterior approach is that it has a statistically higher dislocation rate. Most dislocations of the hip joint are posterior, and this approach disrupts the posterior capsule and muscles that help keep the joint in place. In order to keep the dislocation rate low, it becomes necessary to insert larger femoral heads, and in order to use the largest heads, the surgeon then becomes tempted to use thin metal-only shells on the acetabulum. The posterior approach surgery has been the driving force behind large metal-on-metal hip bearings and all the problems associated with those.
The other commonly performed hip approach, the anterolateral approach, has a statistically lower dislocation risk. The anterolateral approach's major problem is prolonged limping after surgery. Patients sometimes limp for a year, sometimes for ever, when this could have been avoided.
The anterior approach
To address the limping from the anterolateral approach, and the higher dislocation rate with the posterior approach, the direct anterior approach has been popularized by Dr Joel Matta, who is perhaps the most experienced acetabular and pelvic orthopedic surgeon in the US.
The direct approach implies going between (as opposed to through) the muscles and the tendons of the hip. This approach therefore is muscle sparing.
A special orthopedic table is used during surgery.
The patient is positioned with the legs secured in "ski boot" holders and the table allows secure manipulation and appropriate positioning of the hip joint during the surgery.
The table allows safe manipulation of the hip joint. In addition, duing surgery patient is positioned flat on his or her back, and it is easy to get good xrays and confirm position of the prosthesis before surgery is over.
While the incision is smaller and the muscles are treated with more respect, the rest of the operation is still the same: power saws and power reamers are used inside the body to cut and shape the bones for the artificial implant: In the picture below the tool in my left hand is a sterile power saw. I was doing a right hip replacement. This instrument is not too different from the Dremel tools that you can buy at the home improvement store.
Here's a picture of an arthritic eburnated femoral head that has been cut out, soon to be replaced with an artificial piece.
Again, a major advantage, at least the way I see it, is that the procedure is performed with the patient on his or her back, allowing the surgeon to use xray during surgery. For instance, in the picture below, as I am inserting the acetabular cup, I can see that I need to slightly adjust the position of the acetabular component.
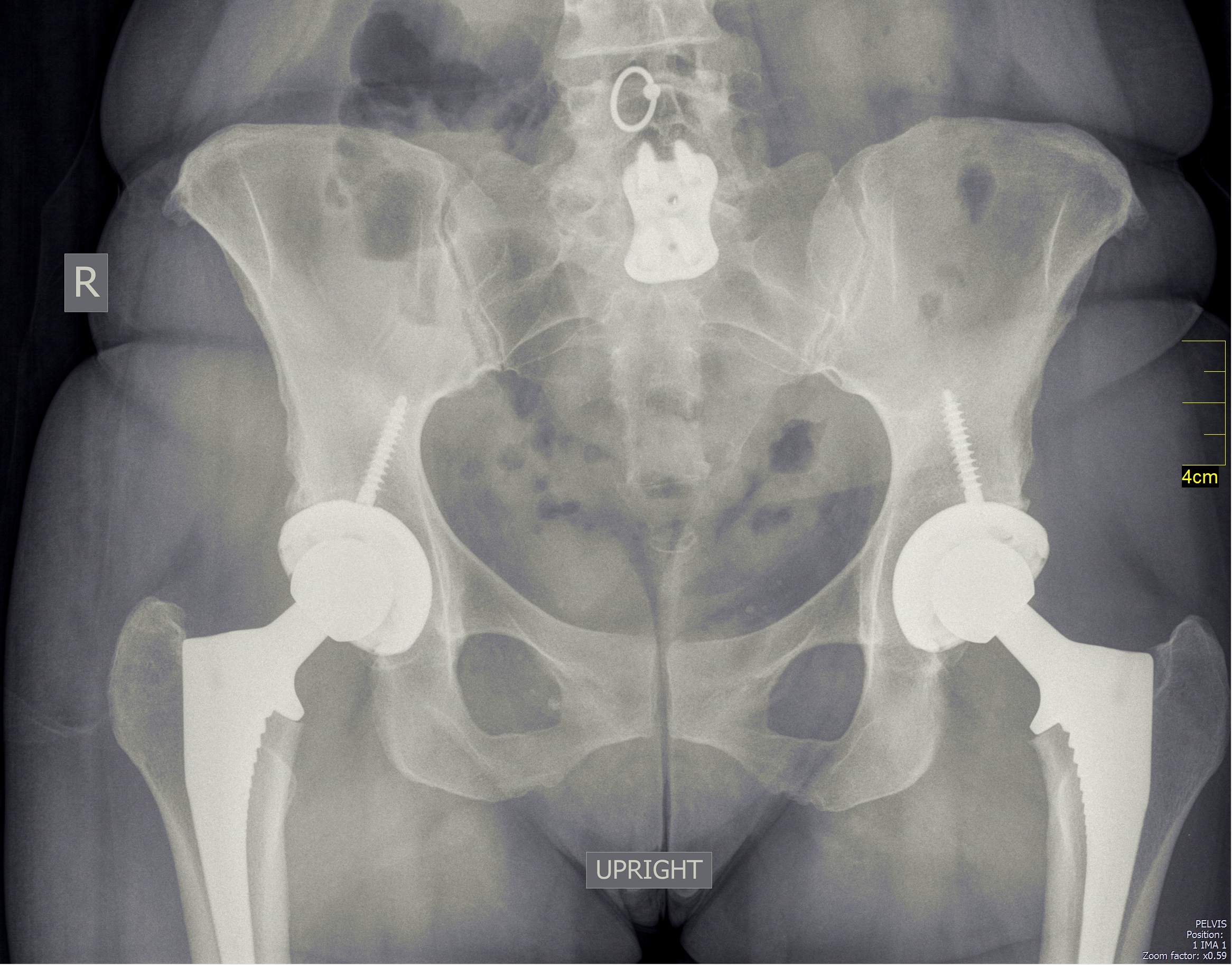
Here, thanks to my cell phone, is the xray appearance of a patient who had both hips replaced:
And here is a video of one of the patients 2 weeks after hip replacement: this sort of fast recovery after a hip replacement sounds unbelievable, and it shows the potential of the anterior approach to the hip.
It is important to remember that for the full potential of this operation to be realized, the patient should be relatively fit. The muscles around the hip should be in good shape, heart and lungs should also be relatively healthy. This operation is a hip replacement and a hip replacement only, and it will not cure the other ailments that may be contributing to a patient's immobility.